Issue: January-March 2016 (Volume-5, Number-1)
Review Article :
Managing Pain in Children
Introduction:
Not only pain but also the anxiety it generates are of due concern to the child, parents as well as the Pediatrician. Providing relief remains as a formidable challenge. The consideration to administer an agent to provide relief of a discomfort precipitates physiologic instability. Chance of serious side effects also causes a novice to avoid an agent or use it only when symptoms are severe. Drugs therapy and its rigid protocol at times lead to unnecessary medication too.
Certain misconceptions about pain are: 1. Children have higher tolerance to pain.
2. Neonates do not perceive pain.
3. Pain perception is decreased because of poor maturity.
4. Children have little or no memory of painful experience.
5. Children have a higher risk for addiction to narcotics, hence best avoided.
In contrast, pain has a very powerful impact on the neuro-behavioural outcome neonates and children.
Few painful procedures commonly performed on children during hospital stay :
| Diagnostic | Therapeutic |
| Arterial sampling | Bladder catheterization |
| Lumbar puncture | Central line insertion / removal |
| Ophthalmic examination (eg. ROP screening) | Chest tube insertion / removal Feeding tube insertion / removal |
| Suprapubic bladder tap | Chest physiotherapy |
| Venipuncture | Dressing change |
Methods used for pediatric pain monitoring:
Infant / Toddler : Various scoring systems are available including : PIPP (Premature Infant Pain Profile); NFCS (Neonatal Facial Coding Scale); NIPS(Neonatal Infant Pain Scale); CRIES (Cry, Requires Oxygen,Increased Vital Signs, Expression, Sleeplessness); N-PASS (Neonatal Pain Agitation and Sedation Scale); and EchelleDouleurinconfortnouveau-neBehaviour . All these are observational scores and we may choose one best suited to us.
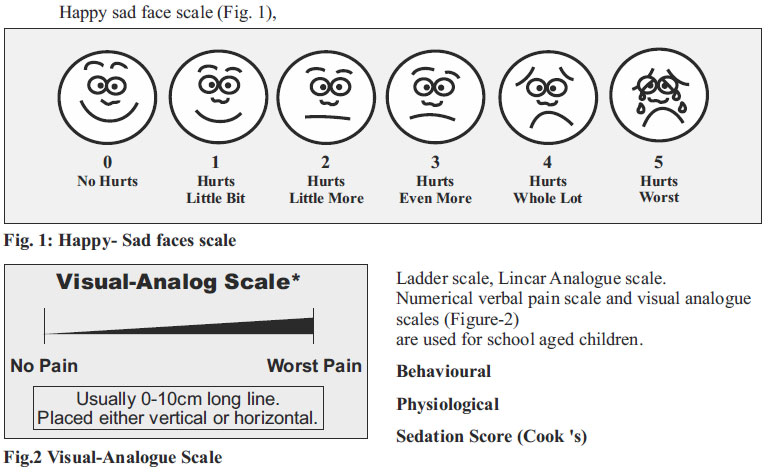
Preschool, school age and adolescent -
Self reporting :
Non-pharmacological ways to reduce pain General guidelines:
- As you would with any person before starting care-Softly greet/talk to the baby before touching- at the onset of any handling or procedure
- Use gentle but still, firm touch rather than light touches or tapping when touching a preterm. For close to term sick neonates- observe their response to light touch and if they display a stress response try the still firm touch.
- Sometimes when a young preterm baby is stressed by an experience just taking a brief break from the care to allow time without stimulation can help the baby to regain a calmer state.
Interventions for stress and pain (nonpharmacological)
*Following interventions are cautiously undertaken when baby is considered medically able to tolerate and age appropriate:
Facilitated tuck (also called containment):
Facilitated Tuck: "Involves firmly containing the infant using a care-giver's hands on both head and lowerlimbs to maintain a 'folded-in' (flexion) position. Infant may or may not be wearing clothes", can be done prior to and during care and procedures that are known or observed to be stressful to the baby.
Swaddling (sometimes called bundling):
"Swaddling is when an infant is securely wrapped in a blanket to prevent the child's limbs from moving around excessively." Swaddling helps a baby achieve the "folded in" or flexion posture achieved through facilitated tuck. Swaddling has been found effective for stable preterm infants for reactivity (stress responses) and immediate regulation of pain.
Swaddling must be used with great caution for sickor very preterm babies because it also restricts access in emergency situations
Kangaroo Care (KC) (also known as skin-to-skin contact):
Infants are placed and held against a caregiver's (usually parent) bare chest during KC. For preterm babies, KC is effective to manage pain reactivity and to support immediate pain-related regulation during stressful or routine painful procedures.
Non-Nutritive Sucking (NNS):
A pacifier or non-lactating nipple- (after breast milk is expressed) is placed into an infant's mouth to stimulate sucking behaviours. NNS has been determined to be effective for preterm babies for pain reactivity and to support immediate painrelated regulation. NNS is also considered effective for immediate pain-related regulation in neonates . Can be used for soothing the stressed infant, and also prior to and during a painful event
Oral sucrose:
Sucrose for analgesia: 0.012 g to 0.12 (0.05 ml to 0.5ml) of 24% solution given orally 2 minutes prior and just prior to painful procedures is suggested for infants on the NICU, especially in combination with other non-pharmacological pain management techniques (i.e. facilitated tuck, NNS) Sucrose procedures has been found to attenuate moderate pain in preterm babies.
Also tending to proper care and handling practices - asper gestational age- also is important to manage stress and pain.
Breast feeding (age appropriately):
As appropriate for the circumstance, breast feeding is as effective as oral sucrose for managing pain in preterm babiesiii
- Cluster cares; allow times for undisturbed rest (protected sleep).
- But not too many stressful interventions to gether.
- If baby is stressed - stop and provide 'time out'
- During care use slow controlled gentle handling/movement. Avoid abrupt changes in position
- Avoid temperature and postural stress- i.e. swaddle in a blanket for weighing and subtract the weight of the blanket from the total on the scale for the baby's weight
- Adjust to promote rest and sleep, establish healthy sleep rhythm
- Lighting: Minimize light where able
- Protect eyes from bright light
- Dim lights at night if safe
- Sound: Range -40-45 dB in NICU
Other Sensory:
- Touch (infant massage)
- Music and Sound: recommend caregiver, and especially, maternal vocals
- Vestibular (movement): recommend KMC and proper care related movement.
Drugs used for pain relief are:
1. Sedative: Drug that reduces excitement.
2. Hypnotic: Provides sleep resembling natural sleep.
3. Analgesic: Relieves pain without causing loss of consciousness.
The goals are:
1. Protect patient's welfare and safety.
2. Minimize physical and mental discomfort
3. Prevent negative physiological effect, treat and maximize amnesia
4. Behaviour modification
5. Safe and early discharge.
Sedation:
A. Controlled Sedation:
Drugs used are- Trichlorofos, Anihistamines and Benzodiazepines.
The goal is to achieve a state of lower consciousness in a controlled manner, preserving protective reflexes, while retaining child's ability to maintain airway, permitting appropriate response to physical stimulation or verbal command. The indications are:
1. Combative child
2. Respiratory distress
3. Pediatric I.C.U. Patients to allay environmental anxiety
4. Minor invasive procedures.
B. Deep sedation:
Drugs used are Opioids (Morphine, Fentanyl), Barbiturates, Benzodiazepines, Ketamine.
Deep sedation is a medically controlled state of depressed consciousness or unconsciousness from which the patient is not easily aroused. It may be accompanied by a partial or complete loss of protective reflexes. It includes inability to maintain a patient's airway independently and respond purposefully to physical stimulation or verbal command.
Indications for deep sedation
1. E.T. intubation - Opioids (Morphine)
2. Patients on ventrilator and Advanced life support
3. Painful procedures: Chest tube placement, venous cut down etc.
4. During CT, MRI and other invasive imaging procedures
5. Endoscopy, Bronchoscopy,
6. Bone marrow, liver and kidney biopsy.
The Anaesthesia Ladder:
The concept of an 'analgesic ladder' has been employed in the management of both adult and pediatric pain associated with cancer. It will help understanding the use of analgesics. It involves a stepwise approach to the management of pain, tailoring the medications to be specific to the needs of the patient. To minimise side effects, the paediatrician usually begins with less potent analgesic and gradually adds or replaces agents until desired amount of analgesia is achieved. In other words, the very circumstances dictate advancing (Step-up) or descending (Step-down) on the ladder path more rapidly than usual or skipping several steps together.
Which is an ideal sedative?
An ideal sedative should have the following characteristics:
1. Rapid onset
2. Predictable duration of activity
3. No active metabolites
4. Effects dissipate rapidly when agent is discontinued
5. Multiple options for route of delivery
6. Easy to titrate by continuous infusion
7. Limited effects on cardio-respiratory function
8. Effects and duration not altered by renal or hepatic disease
9. No interference with effects or metabolism by other drugs
10. Wide therapeutic index.
Pre-sedation protocol:
1. Candidates for sedation: Eligibility criteria need to meet.
2. Pre-sedation physical examination for medical problems
3. Risk-benefit of sedation well explained to parents followed by written, informed consent
4. Nil Per oral guidelines:
- 4 hrs for infants < 6 months for formula
- 6 hrs for infants > 6 months for formula
- 2 hrs for clear liquid at any age
Equipments require priop to administration of sedation:
Before embarking on planned sedation ensure availability of the following on patient's bed side.
1. Positive pressure oxygen delivery system able to deliver > 90% O2.
2. Appropriate sizes masks and oral airways.
3. Suction apparatus with catheters
4. Monitors for :
- Oxygen: Pulse oxymetry
- Blood Pressure
- H.R. (Pulse Oxymetry or ECG)
- Temperature (Thermometer)
Drugs used for sedation and analgesia:
A. Sedative agents ;
1) Benzodiazepines - Effective t/2 > 24 hrs. - Diazepam, Flurazepam
Effective t/2 5-24 hrs. - Nitrazepam, Lorazepam
Effective t/2 < 5 hrs - Midazolam, Trazolam
2) Chloral Hydrate - Trichlorofos
3) Barbiturates< - Pentobarbital, Thiopentel
4) Anti Histamines - Promethezine - Trimethazine
5) Newer agent - Propofol
B. Analgesic agents:
1. Natural - Morphine, codeline
2. Semisynthetic - Heroin, Diphenhydramorphine
3. Synthetic - Butorphanol, Pethidine, Methadone, Pentazocin, Fentanyl, Acfentanil
b) Non-opioid Analgesics:
1. Ketorolac, Indomethecin, Paracetamol, Ibuprofen
2. Tricylic antidepressants, Imipramine, Amitriptyline
c) Sedation and analgesic agents :
1. Opiates
2. Ketamine
3. Combination of drugs:
- Lytic cocktail (DTP) - Midazolam + Fentanyl
d) Anasthetic agents: 1) Regional / Local :Lidocaine, Bupivacaine
2) Topical - TAL lotion, EMLA cream
3) Inhalational anesthetic agents _ Nitrous Oxide
Criteria for discharge after sedation:
1) Cardiovascular function and airway patency should be stable.
2) Protective reflexes should be intact and patient is arousable.
3) The patient can talk (if age appropriate)
4) The patient can sit up (if age appropriate)
5) For handicapped child with developmental delay; return to pre-sedation level of consciousness.
6) The state of hydration is adequate.
Complications of sedation:
1. Respiratory system : Upper airway obstruction - Central respiratory depression (Hypoventilation)
2. Cardiovascular - Hypotension, Cardiovascular depression
3. Delayed awakening
4. Paradoxical agitation
5. Paralytic ileus
6. Immunosupression
7. Hepatic and renal dysfunction
8. Hazards of immobility - muscle wasting, venous thrombosis, pressure sores
Regional approaches in children:
Whenever it is necessary to sedate a child one must consider:
1. The type of procedure planned (painful or non painful)
2. The duration of the procedure.
3. The underlying medical condition of the patient
4. The need for anxiolysis or narcosis.
5. Experience with alternative techniques or route of administration.
6. Sedation and procedures should not be done by one individual - two persons are needed.
7. Informed consent should be taken prior to procedure.
8. Fasting guidelines must be followed.
9. Monitoring during pre, intra and post procedure period
10. Combination of dug use is at risk - (Benzodiazepine + Local anesthetic is associated with increased seizure threshold, Benzodiapine + Opioid associated with apnoea).
Some specific uses of analgesia:
IV insertion
Topical anaesthetic cream for 30-45 mins; distraction eg dolls, oral sucrose combined with non-nutritive sucking for infants under three months.
Lumbar puncture
Topical anaesthetic cream for 30-45 mins, 1 % lignocaine with 25G needle.
Oral sucrose combines with non-nutritive sucking for infants under 3 months.
Removal of nasal/pharyngeal foreign body
Topical phenylephrine (0.5%) & lignocaine spray (Cophenylcaine) or nebulised lignocaine (1.0%) 1 ml in 3 ml 0.9% NaCl.
Earache
Topical aural analginotic drop (Onset in 10 minutes) or 1% Lignocaine 2 drops.
Eye
Topical amethocaine 0.5% to examine; patch +/- atropine (to reliever iris spasm) Oral sucrose combined with non-nutritive sucking for infants under three months.
Regional anaesthesia (Bier's block): As given in I.V. Regional Anaesthesia.
Systemic analgesia - see nitrous oxide section below.
Doses of common analgesics:
Paracetamol: 15-20 mg/kg (max 90 mg/kg/day) orally or PR
Non Steroidal Anti-Inflammatory Drugs:
Naproxen 5-10 mg/kg (max 500 mg) 12-hrly orally or PR
Ibuprofen 2.5 - 10 mg/kg (max 600 mg) 6-8 hrly oral
Opioids:
Codeine 0.5 - 1 mg/kg orally (as adjunct - sedation)
Pethidine 1mg/kg i.m. Or 0.25 - 0.5 mg/kg/i.v.
Morphine 0.1 mg/kg i.m. or 0.05 - 0.1 mg/kg i.v.
Midazolam
Oral/buccal 0.5 - 1.0 mg/kg. (max 15 mg)
Intranasal 0.6 mg/kg (max 10 mg) - may have more rapid onset.
Ketamine IV: (with local anaesthetic cream)
Especially useful for procedures longer than 15-20 minutes.
The Ketamine dose of 1-1.5 mg/kg is given slowly over (1-2 min) as more rapid administration is associated with respiratory depression.
Further incremental doses of 0.5 mg/kg may be given if sedation is inadequate or longer sedation is necessary.
Atropine and Midazolam may be given prior to or with the Ketamine.
IM Ketamine can be safely used without i.v. access.
3-4 mg/kg Ketamine with atropine and Midazolam mixed in the same syringe.
A repeat dose of 2-4 mg/kg may be given after 10 minutes if sedation is inadequate.
Summary:
A "Cook Book" approach to analgesia and sedation is impossible because of the diversity of patients and clinical scenarios. When amnesia is required benzodiazepine infusion can be used. When analgesia is required opioid infusion or using PCA device (Morphine, Fentanyl) is safe. When benzodiazepines and opioid are ineffective or associated with cardiovascular depression, the alternatives are ketamine or pentolbarbital. Non opioid analgesic is used to decrease the side effects of oral drugs. Regional or local anesthesia can be used to decrease the local painful situations. With improved capability of monitoring, more potent drugs and better understanding of pharmacokinetics in childhood, it is possible to provide better care in a safe and caring atmosphere.
Recommendations
- Recognize and assess pain, documenting in the patient's chart.
- Use non-pharmacologic and pharmacologic strategies to reduce pain experience preoperatively.
- Be familiar with the patient's medical history to avoid prescribing a drug that would be otherwise contra- indicated.
- Comprehend the consequences, morbidities, and toxicities associated with the use of specific therapeutics.
- Consider non-opioid analgesics as first line agents for pain management.
- Utilize drug formularies in order to accurately prescribe medications for the management of postoperative pain.
- Consider combining NSAIDs with acetaminophen to provide a greater analgesic effect than the single agent alone.
Sources of support: None Declaration on competing interests: None Funding: None
References:
1. Combine opioid analgesics with NSAIDs for post-operative treatment of moderate to severe pain in children and adolescents. K. J. S. Anand and the international evidence based groupfor neonatal pain. Consensus statement for the preventionof pain in the newborn. Arch PediatrAdolesc Med 2000;155: 173-80
2. Fern, D. (2011). A neurodevelopmental care guide topositioning and handling the premature, fragile, or sickinfant. New York: DF Publishing.
3. Riddell, P., Racine, N., &Turcotte, K. e. (2012). Non-Pharmacological management of infant and young childprocedural pain. Cochrane Database of Systematic Reviews, 10:CD006275.
4. Spruill, C., &LaBrecque, M. A. (2012). Chapter 67: Preventing and treating pain and stress among infantsin the newborn intensive care unit. In J. P. Cloherty, E. C.Eichenwald, A. R. Hansen, & A. R. Stark, Manual of neonatalcare, seventh edition (7th ed., pp. 870- 885). Philadelphia:Lippincott Williams and Wilkins, a Wolters Kluwer business.
5. Cignaccio, E. L., Sellam, G., Stoffel, L., Gerull, R., Nelle, M.,Kanwaljeet, J., &Engberg, A. a. (2012). Oral sucrose and"facilitated tucking" for repeated pain relief in preterms:A randomized control trial. Pediatrics, DOI: 10.1452/peds.2011-1879.
6. WHO: model formulary for children. Geneva, World Health Organization, 2010.
NIJP : Vol.-5, No.-1



